Raynaud’s Disease Medicines:-
Understanding Raynaud’s Disease and Its Management:-
Raynaud’s disease, also known as Raynaud’s phenomenon or Raynaud’s syndrome, is a condition that affects blood flow to certain parts of the body—typically the fingers and toes. During episodes, small blood vessels narrow in response to cold temperatures or emotional stress, temporarily limiting blood circulation to affected areas. This causes the skin to change color (often turning white, then blue, then red as blood flow returns) and may result in numbness, tingling, or discomfort. While the condition itself is not typically dangerous, it can significantly impact daily comfort and quality of life. Medical management focuses on improving blood flow, reducing episode frequency and severity, and preventing potential complications.
Types of Medications Available:-
The Raynaud’s disease category includes various medication types that work to improve circulation and manage symptoms:
Calcium Channel Blockers: These medications help relax and widen blood vessels by preventing calcium from entering cells in the vessel walls. They are among the most commonly prescribed options for Raynaud’s and work to reduce the frequency and severity of vasospastic episodes.
Vasodilators: This group of medications directly causes blood vessels to expand and relax, improving blood flow to extremities. Different vasodilators work through various mechanisms to achieve this effect.
Phosphodiesterase Inhibitors: These medications promote blood vessel relaxation and improved circulation, particularly in cases where other treatments have not provided sufficient relief.
Alpha-Blockers: These work by blocking certain receptors that cause blood vessels to constrict, potentially helping to keep small blood vessels open during cold exposure or stress.
Topical Preparations: Some formulations are applied directly to affected areas to promote local blood vessel dilation and improved circulation.
Antiplatelet Medications: In certain situations, medications that reduce blood clotting may be considered to improve blood flow, particularly in more severe cases.
General Usage and Treatment Approach:-
Medications for Raynaud’s disease are used as part of a comprehensive management strategy that typically includes lifestyle modifications alongside pharmaceutical treatment. These medications require prescriptions and medical oversight because:
– Treatment selection depends on symptom severity, frequency of episodes, and whether the condition is primary (occurring on its own) or secondary (associated with another health condition)
– Response to treatment varies among individuals, often requiring adjustments to find the most effective approach
– Some medications used for Raynaud’s also affect blood pressure and heart function, necessitating careful monitoring
– Dosing may need modification based on individual tolerance, other health conditions, and concurrent medications
– Treatment goals focus on symptom control rather than cure, as Raynaud’s is typically a chronic condition
Many people with Raynaud’s find that medication works best when combined with practical measures such as keeping warm, avoiding sudden temperature changes, managing stress, and protecting extremities during cold exposure.
Promoting Safe Medicine Awareness:-
Medical Supervision Required: All medications for Raynaud’s disease require prescriptions and should only be used under healthcare provider guidance. Self-diagnosis and self-treatment can lead to inappropriate medication use or delayed diagnosis of underlying conditions.
Individual Response Varies: What works well for one person may not be effective or tolerable for another. Healthcare providers often try different options or combinations to find the most suitable approach for each individual.
Gradual Adjustments: Many of these medications require gradual dose increases or decreases. Never change your dosing schedule or stop taking medication abruptly without consulting your healthcare provider.
Monitoring Needs: Regular follow-up appointments help assess treatment effectiveness, monitor for side effects, and make necessary adjustments. Blood pressure monitoring may be particularly important with certain medication types.
Interaction Awareness: These medications can interact with other prescriptions, over-the-counter products, supplements, and certain foods or beverages. Always inform all healthcare providers about everything you’re taking.
Lifestyle Integration: Medication effectiveness often improves when combined with protective measures such as layered clothing, heated gloves, stress management techniques, and avoiding smoking.
Exploring Treatment Options Confidently:-
When considering medications for Raynaud’s disease, helpful approaches include:
– Having detailed discussions with healthcare providers about symptom patterns, severity, and impact on daily activities
– Understanding that finding the right medication may take time and patience
– Keeping records of episode frequency, triggers, and duration to help assess treatment effectiveness
– Asking questions about how medications work, potential side effects, and what to expect during treatment
– Being open about lifestyle factors, other health conditions, and treatment preferences
– Discussing both medication and non-medication strategies for comprehensive symptom management
– Seeking specialist consultation (rheumatology or vascular medicine) when primary care approaches aren’t providing adequate relief
Informed decision-making involves understanding your options while working collaboratively with healthcare professionals who can evaluate your specific situation and guide appropriate treatment choices.
Frequently Asked Questions
1. What’s the difference between primary and secondary Raynaud’s, and does it affect medication choices?
Primary Raynaud’s occurs on its own without an underlying disease and is generally milder. Secondary Raynaud’s is associated with other conditions such as autoimmune diseases, connective tissue disorders, or vascular problems, and tends to be more severe. This distinction significantly affects treatment approaches. Primary Raynaud’s often responds well to lifestyle modifications alone, with medication reserved for more bothersome cases. Secondary Raynaud’s more frequently requires medication because episodes may be more severe and carry greater risk of tissue damage. Healthcare providers also consider treating the underlying condition in secondary Raynaud’s. The medication types and intensiveness of treatment typically differ based on whether the condition is primary or secondary, which is why proper medical evaluation is essential before starting any treatment.
2. How quickly do Raynaud’s medications start working, and how long until full effectiveness?
The timeframe varies depending on the medication type and individual response. Some vasodilators may provide noticeable improvement within days to a couple of weeks, while others, particularly calcium channel blockers, might require 2-4 weeks of consistent use before full benefits become apparent. It’s important to understand that these medications work preventively—they reduce the frequency and severity of future episodes rather than stopping an episode in progress. During initial treatment, healthcare providers typically start with lower doses and gradually increase as needed, which means achieving optimal symptom control may take several weeks to months. Patience during this adjustment period is important. If no improvement occurs after an adequate trial period, healthcare providers may try different medications or combinations. Effectiveness should be evaluated over time by tracking episode frequency, duration, and severity.
3. Can I stop taking Raynaud’s medication during warmer months when symptoms improve?
This is a common question since many people experience seasonal variation in symptoms, with fewer or no episodes during warm weather. The answer depends on several factors i, including medication type, symptom severity, whether Raynaud’s is primary or secondary, and individual circumstances. Some healthcare providers may support seasonal adjustments, while others recommend year-round treatment for consistent vascular health, particularly in secondary Raynaud’s. Certain medications should never be stopped abruptly due to potential rebound effects or withdrawal issues. If you’re considering seasonal medication changes, this discussion should happen proactively with your healthcare provider well before warmer weather arrives. They can provide guidance on whether seasonal adjustment is appropriate, how to safely taper if stopping temporarily, and when to restart treatment as temperatures drop. Never make these decisions independently.
4. What side effects should I be aware of with Raynaud’s disease medications?
Side effects vary by medication class. Calcium channel blockers commonly cause headaches, dizziness, flushing, ankle swelling, and fatigue, particularly when starting treatment or increasing doses. Vasodilators may cause similar effects, plus potential heart palpitations. Blood pressure lowering is common with several medication types, which can lead to lightheadedness, especially when standing quickly. Some people experience digestive upset, including constipation or nausea. Headaches are particularly common initially but often improve with continued use. Most side effects are mild to moderate and may diminish as your body adjusts to the medication. Serious side effects are less common but require immediate medical attention—these include severe dizziness, fainting, irregular heartbeat, or significant swelling. Your healthcare provider can discuss specific side effects related to your prescribed medication and provide strategies for managing common ones. If side effects become problematic, medication adjustments or alternatives are often available rather than discontinuing treatment entirely.
Disclaimer:-
This content is provided for educational purposes only and does not constitute medical advice. Raynaud’s disease requires proper medical evaluation and individualized treatment planning. Always consult qualified healthcare professionals for diagnosis, treatment recommendations, and personalized guidance regarding your specific condition.
-
Cholergol 30 Mg (Nicergoline)
Active Ingredient Nicergoline Manufacturer Inga Laboratories Pvt Ltd Packaging 10 Tablets in Strip Strength 30 Mg Delivery Time 6 to 15 days SKU: Cholergol 30 Mg (Nicergoline) Price range: $116.00 through $340.00Cholergol 30 Mg (Nicergoline)
Price range: $116.00 through $340.00 -
Minipress XL 2.5 Mg (Prazosin)
Active Ingredient Prazosin Manufacturer Pfizer India Ltd Packaging 30 tablets in 1 strip Strength 2.5 Mg And 5 Mg Delivery Time 6 To 15 days SKU: Minipress XL (Prazosin) Price range: $37.00 through $115.00Minipress XL 2.5 Mg (Prazosin)
Price range: $37.00 through $115.00 -
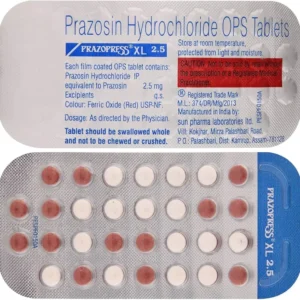
Prazopress XL 2.5 Mg (Prazosin)
Active Ingredient Prazosin Manufacturer Sun Pharmaceutical Industries Ltd Packaging 30 tablets in 1 strip Strength 2.5 Mg Delivery Time 6 To 15 days SKU: Prazopress XL 2.5 Mg (Prazosin) Price range: $27.00 through $80.00Prazopress XL 2.5 Mg (Prazosin)
Price range: $27.00 through $80.00