Psoriatic Arthritis Medicines:-
Understanding Psoriatic Arthritis Treatment:-
Psoriatic arthritis is a chronic inflammatory condition that affects both the joints and the skin, combining features of arthritis with the skin condition psoriasis. This complex autoimmune disease causes joint pain, stiffness, and swelling, along with characteristic skin patches and changes. The condition varies significantly in severity and presentation among individuals, requiring personalized treatment approaches that address both joint inflammation and skin symptoms.
Pharmaceutical management plays a central role in controlling disease activity, preserving joint function, reducing inflammation, and improving overall quality of life. The medications available for psoriatic arthritis have expanded considerably in recent years, offering multiple therapeutic pathways to manage this multifaceted condition.
Types of Medications Available:-
The psoriatic arthritis category includes several medication classes, each targeting different aspects of the inflammatory process:
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These medications help reduce pain and inflammation in the joints. They work by blocking enzymes that produce inflammatory substances in the body and are often used for symptom management, particularly in milder cases or alongside other treatments.
Disease-Modifying Antirheumatic Drugs (DMARDs): This category includes conventional synthetic DMARDs that work throughout the immune system to slow disease progression and prevent joint damage. These medications typically take several weeks to months to show full effectiveness.
Biologic Therapies: These advanced medications are engineered proteins that target specific components of the immune system involved in inflammation. Different biologics target different inflammatory pathways, including tumor necrosis factor (TNF) inhibitors, interleukin inhibitors, and T-cell modulators.
Targeted Synthetic DMARDs: Newer oral medications that work by blocking specific enzymes inside immune cells that contribute to inflammation, offering another treatment option with a different mechanism of action.
Corticosteroids: Short-term anti-inflammatory medications that can rapidly reduce inflammation and symptoms. These are typically used for limited periods or as bridge therapy while waiting for other medications to take effect.
Topical Treatments: Medications applied directly to the skin to manage psoriasis patches that often accompany the joint symptoms.
General Usage Considerations:-
Medications for psoriatic arthritis require prescription authorization and ongoing medical supervision. Treatment approaches typically involve:
– Starting with one medication and potentially adding others if disease activity continues
– Regular monitoring through blood tests, physical examinations, and imaging studies
– Gradual dosage adjustments based on individual response and tolerance
– Combination therapy using multiple medication classes to address different aspects of the disease
– Long-term commitment, as these are chronic condition management medications rather than short-term solutions
Healthcare providers consider numerous factors when developing treatment plans, including disease severity and pattern, which joints are affected, presence and extent of skin involvement, patient age and overall health, other existing medical conditions, lifestyle factors, and previous treatment responses. Treatment goals focus on reducing inflammation, preventing joint damage, managing pain, improving physical function, and addressing skin symptoms.
Safe Medicine Awareness:-
Medical Supervision: All psoriatic arthritis medications should be taken under the guidance of qualified healthcare providers, typically rheumatologists or dermatologists with experience managing this condition. Self-medication is not appropriate for these prescription treatments.
Infection Monitoring: Many psoriatic arthritis medications affect immune system function, which can increase susceptibility to infections. Patients should be vigilant about signs of infection and maintain recommended vaccinations, though the timing of certain vaccines may need coordination with treatment schedules.
Regular Health Monitoring: Ongoing blood tests and health assessments are necessary to monitor medication effectiveness and detect potential side effects early. Some medications require specific screening before initiation and periodic monitoring during treatment.
Drug Interactions: These medications may interact with other prescriptions, over-the-counter products, herbal supplements, and even certain vaccines. Complete disclosure of all medications and supplements to healthcare providers is essential.
Pregnancy and Family Planning: Many psoriatic arthritis medications have implications for pregnancy and breastfeeding. Individuals of childbearing potential should discuss family planning with healthcare providers well in advance.
Proper Storage and Handling: Some medications, particularly biologics, require refrigeration and careful handling. Following storage instructions ensures medication effectiveness and safety.
Making Informed Decisions:-
When considering psoriatic arthritis treatment options:
– Engage in detailed conversations with rheumatology specialists about the full range of available therapies
– Understand that finding the most effective treatment may involve trying different options
– Ask about the expected timeline for improvement, as some medications work gradually
– Discuss potential side effects and strategies for managing them
– Consider lifestyle factors such as administration method (oral vs. injection vs. infusion)
– Inquire about medication costs, insurance coverage, and patient assistance programs
– Learn about the importance of adherence to prescribed regimens for optimal outcomes
– Connect with patient support resources and educational materials
Treatment decisions should always be made collaboratively with qualified healthcare professionals who can assess your specific disease characteristics, medical history, and individual needs.
Frequently Asked Questions?
1. What is the difference between biologics and traditional DMARDs for psoriatic arthritis?
Traditional DMARDs (disease-modifying antirheumatic drugs) are typically small-molecule medications taken orally that work broadly throughout the immune system to reduce inflammation and slow disease progression. They’ve been used for decades and include medications that affect multiple immune pathways. Biologics, by contrast, are larger protein-based medications created using biotechnology that target very specific components of the immune system, such as particular inflammatory proteins or immune cells. Biologics are usually administered by injection or infusion rather than orally. While traditional DMARDs often take weeks to months to show full effects, biologics may work somewhat faster in some cases. Both types can be highly effective, and the choice between them depends on disease severity, specific symptoms, previous treatment responses, individual health factors, and practical considerations like administration preferences.
2. How long does it take for psoriatic arthritis medications to start working?
The timeline for symptom improvement varies considerably depending on the medication type. NSAIDs typically provide symptom relief within hours to days, but don’t address underlying disease progression. Traditional DMARDs generally require 6 to 12 weeks before noticeable improvement occurs, with full benefits sometimes taking 3 to 6 months. Biologic medications may begin showing effects within 4 to 12 weeks, though response time varies among individuals and different biologics. Targeted synthetic DMARDs often demonstrate effects within 2 to 3 months. Corticosteroids work quickly, often within days, but are typically used for the short term. Because of these varying timelines, healthcare providers may prescribe faster-acting medications for symptom control while waiting for slower-acting disease-modifying treatments to reach full effectiveness. Patience and consistent medication adherence during this initial period are important for optimal outcomes.
3. Do psoriatic arthritis medications treat both joint and skin symptoms?
The ability of medications to address both joint and skin manifestations varies by medication class. Many biologic therapies effectively treat both aspects of psoriatic arthritis, targeting inflammatory pathways that contribute to both joint inflammation and skin lesions. Some biologics are particularly effective for skin symptoms while also helping joints, while others primarily target joint inflammation. Traditional DMARDs primarily focus on joint disease but may provide some skin benefits. Targeted synthetic DMARDs can help both manifestations to varying degrees. In some cases, patients may need separate medications for optimal management of skin and joint symptoms, such as combining a joint-focused DMARD with topical treatments for psoriasis. Healthcare providers consider the severity and extent of both skin and joint involvement when selecting treatments, aiming to address the complete disease picture with the most appropriate medication regimen.
4. Are there lifestyle factors that affect how well psoriatic arthritis medications work?
Several lifestyle factors can influence medication effectiveness and overall disease management. Maintaining a healthy weight is particularly important, as excess weight can reduce response to some medications and increase joint stress. Smoking has been associated with poorer treatment outcomes and may reduce the effectiveness of certain biologic therapies. Regular physical activity, within comfortable limits, helps maintain joint flexibility and overall health, complementing medication effects. Stress management is relevant since stress can trigger disease flares. Adequate sleep supports immune system regulation and overall well-being. Alcohol consumption should be discussed with healthcare providers, as it may interact with some medications or affect liver function, which is monitored during treatment. A balanced diet rich in anti-inflammatory foods may support overall health. Following medication schedules precisely as prescribed, without skipping doses, maximizes treatment effectiveness. These lifestyle factors work synergistically with medications rather than replacing them.
Disclaimer:-
This information is provided for educational purposes only and does not constitute medical advice. Always consult qualified healthcare professionals for personalized diagnosis, treatment recommendations, and medical guidance specific to your individual health situation.
-
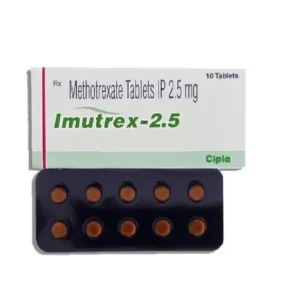
Imutrex 2.5 Mg (Methotrexate)
Active Ingredient Methotrexate Manufacturer Cipla Limited Packaging 10 tablets in 1 strip Strength 2.5 Mg, 7.5 Mg, 10 Mg Delivery Time 6 To 15 days SKU: Imutrex 2.5 Mg (Methotrexate) Price range: $27.00 through $195.00Imutrex 2.5 Mg (Methotrexate)
Price range: $27.00 through $195.00 -
Lefumide 10 Mg (Leflunomide)
Active Ingredient Leflunomide Manufacturer Cipla Limited Packaging 10 tablets in 1 strip Strength 10 Mg Delivery Time 6 to 15 days SKU: Lefumide 10 Mg (Leflunomide) Price range: $28.00 through $201.00Lefumide 10 Mg (Leflunomide)
Price range: $28.00 through $201.00