Rheumatoid Arthritis Medicines:-
Understanding Rheumatoid Arthritis Treatment:-
Rheumatoid arthritis (RA) is a chronic autoimmune condition where the body’s immune system mistakenly attacks the lining of joints, causing inflammation, pain, swelling, and potential joint damage over time. Unlike osteoarthritis, which results from wear and tear, rheumatoid arthritis involves immune system dysfunction that can affect multiple joints symmetrically, often in the hands, wrists, and feet. Managing this condition typically requires medication as a central component of care, alongside lifestyle modifications and regular medical monitoring.
The goal of pharmaceutical treatment for rheumatoid arthritis is to reduce inflammation, slow disease progression, preserve joint function, and improve quality of life. Modern approaches emphasize early and aggressive treatment to prevent irreversible joint damage and disability.
Types of Medications Available:-
The rheumatoid arthritis category includes several medication classes, each serving different purposes in disease management:
Disease-Modifying Antirheumatic Drugs (DMARDs): These medications work to slow the progression of rheumatoid arthritis and prevent joint damage. Conventional DMARDs affect the immune system broadly, while newer targeted synthetic DMARDs focus on specific immune pathways. These are typically considered foundational treatments for RA.
Biologic Response Modifiers (Biologics): These are sophisticated medications produced from living organisms that target specific components of the immune system involved in inflammation. They may block certain proteins or immune cells that drive the inflammatory process in rheumatoid arthritis.
Corticosteroids: Anti-inflammatory medications that can quickly reduce swelling and pain. They may be used short-term during flares or at low doses alongside other treatments to control inflammation while slower-acting medications take effect.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These medications help manage pain and reduce inflammation but do not slow disease progression. They may be used to provide symptom relief in conjunction with disease-modifying treatments.
Pain Relief Medications: Various analgesic options help manage discomfort and improve daily functioning, though they do not address the underlying disease process.
JAK Inhibitors: A newer class of oral medications that block specific enzymes involved in the inflammatory response, offering an alternative for patients who may not respond adequately to other treatments.
General Usage Considerations:-
Rheumatoid arthritis medications are prescription treatments requiring careful medical supervision. Important aspects of their use include:
– Early Initiation: Healthcare providers often recommend starting disease-modifying treatments soon after diagnosis to prevent joint damage
– Monitoring Requirements: Regular blood tests, physical examinations, and sometimes imaging studies help assess treatment effectiveness and monitor for potential side effects
– Combination Approaches: Multiple medications are frequently used together to achieve better disease control
– Gradual Effect: Many RA medications take weeks or months to show their full benefit, requiring patience and adherence
– Individual Response: People respond differently to various treatments, and finding the most effective medication or combination may involve some trial and adjustment
– Long-Term Commitment: Rheumatoid arthritis is a chronic condition, and most treatments are continued indefinitely to maintain disease control
Treatment plans are highly personalized based on disease severity, activity level, prior treatment responses, other health conditions, lifestyle factors, and individual preferences.
Safe Medicine Awareness:-
Medical Supervision: All rheumatoid arthritis medications require prescriptions and ongoing oversight by qualified healthcare providers, typically rheumatologists or other specialists experienced in managing autoimmune conditions.
Adherence Importance: Taking medications as prescribed is crucial for achieving optimal disease control. Missing doses or stopping treatment prematurely can lead to disease flares and progression of joint damage.
Infection Risk: Many RA medications work by modulating the immune system, which can increase susceptibility to infections. Patients should be vigilant about infection prevention and promptly report signs of illness to healthcare providers.
Screening and Vaccinations: Before starting certain RA medications, healthcare providers may conduct screening tests for infections like tuberculosis or hepatitis. Staying current with recommended vaccinations is important, though live vaccines may need to be avoided with some treatments.
Drug Interactions: RA medications can interact with other prescriptions, supplements, and over-the-counter products. Always inform all healthcare providers about every medication and supplement being taken.
Pregnancy and Family Planning: Some RA medications can affect pregnancy or fetal development. Individuals who are pregnant, planning pregnancy, or breastfeeding should discuss this with their healthcare team, as medication adjustments may be necessary.
Reliable Sources: Only obtain medications from licensed, reputable pharmacies to ensure authenticity and proper storage. Counterfeit medications pose serious health risks.
Navigating Treatment Options:-
When exploring rheumatoid arthritis medications, consider:
– Discussing treatment goals and expectations with your rheumatologist
– Understanding the benefits and potential risks of different medication options
– Asking about the timeline for expected improvement
– Learning about potential side effects and how they’re managed
– Inquiring about administration methods (oral, injection, infusion) and choosing what fits your lifestyle
– Understanding cost considerations and insurance coverage
– Exploring patient assistance programs if affordability is a concern
– Joining support groups or educational programs to learn from others’ experiences
– Keeping detailed records of symptoms and medication responses to share with healthcare providers
Effective rheumatoid arthritis management is a collaborative process between patients and healthcare teams, built on open communication, realistic expectations, and shared decision-making.
Frequently Asked Questions?
1. What is the difference between DMARDs and biologics for rheumatoid arthritis?
DMARDs (Disease-Modifying Antirheumatic Drugs) are abroad categoryy that includes both conventional synthetic DMARDs and biologic DMARDs. Conventional DMARDs are typically small-molecule drugs that affect the immune system broadly and have been used for decades. Biologic DMARDs, often simply called “biologics,” are larger, more complex molecules produced using biotechnology from living cells. They target very specific parts of the immune system, such as particular inflammatory proteins or immune cells. Biologics are generally prescribed when conventional DMARDs don’t provide adequate disease control, though sometimes they’re used earlier in aggressive cases. Both types aim to slow disease progression and prevent joint damage, but they differ in how they’re made, how specifically they act, how they’re administered, and their cost profiles.
2. How long does it take for rheumatoid arthritis medications to work?
The timeframe for experiencing benefits varies significantly depending on the medication type. Corticosteroids and NSAIDs may provide symptom relief within hours to days, but they don’t modify disease progression. Conventional DMARDs typically take 6 to 12 weeks before noticeable improvement occurs, with maximum benefit sometimes not apparent until 3 to 6 months. Biologic medications may work somewhat faster, with some people noticing improvement within 2 to 6 weeks, though full effects may still take several months. JAK inhibitors can sometimes show benefits within a few weeks. Because these medications work gradually, healthcare providers emphasize the importance of patience and continuing treatment even when immediate results aren’t apparent. Regular monitoring helps determine whether a medication is working effectively or whether adjustments are needed.
3. Do rheumatoid arthritis medications need to be taken forever?
For most people with rheumatoid arthritis, medication is a long-term or lifelong commitment. Because RA is a chronic autoimmune condition without a cure, stopping disease-modifying medications typically allows the disease to become active again, potentially leading to joint damage and worsening symptoms. Some individuals who achieve sustained remission might work with their healthcare providers to carefully reduce medication doses, but this is done gradually and with close monitoring. Complete discontinuation is rarely recommended, as the risk of disease flare is substantial. The decision about continuing, adjusting, or attempting to reduce medications should always be made collaboratively with rheumatology specialists based on disease activity, treatment response, side effects, and individual circumstances.
4. Can I take over-the-counter supplements alongside my RA medications?
While some people with rheumatoid arthritis use dietary supplements, it’s essential to discuss any supplements with healthcare providers before taking them. Some supplements can interact with RA medications, potentially reducing their effectiveness or increasing side effects. For example, certain herbal supplements may affect how the liver processes medications or may stimulate the immune system in ways that counteract immunosuppressive treatments. Some supplements, like fish oil or turmeric, are sometimes discussed for their potential anti-inflammatory properties, but evidence for their effectiveness in RA varies. Even seemingly harmless vitamins can interact with medications. Healthcare providers and pharmacists can review specific supplements and advise whether they’re safe to use alongside prescribed RA treatments.
Disclaimer:-
This information is educational in nature and does not replace professional medical advice. Consult qualified healthcare providers for personalized diagnosis, treatment recommendations, and ongoing care guidance specific to your individual health situation.
-
Cyclophil Me 25mg (Cyclosporine)
Active Ingredient Cyclosporine Manufacturer Biocon Limited Packaging 5 capsules in 1 strip, 6 capsules in 1 strip Strength 25mg, 50mg, 100mg Delivery Time 6 To 15 days SKU: Cyclophil Me 25mg (Cyclosporine) Price range: $21.00 through $200.00 -
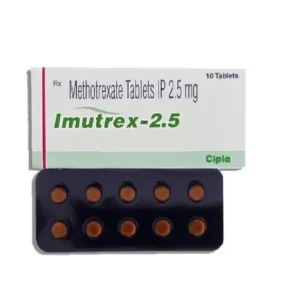
Imutrex 2.5 Mg (Methotrexate)
Active Ingredient Methotrexate Manufacturer Cipla Limited Packaging 10 tablets in 1 strip Strength 2.5 Mg, 7.5 Mg, 10 Mg Delivery Time 6 To 15 days SKU: Imutrex 2.5 Mg (Methotrexate) Price range: $27.00 through $195.00 -
Lefumide 10 Mg (Leflunomide)
Active Ingredient Leflunomide Manufacturer Cipla Limited Packaging 10 tablets in 1 strip Strength 10 Mg Delivery Time 6 to 15 days SKU: Lefumide 10 Mg (Leflunomide) Price range: $28.00 through $201.00